MRI ‘Patterns’ May Aid in Diagnosing Sarcoidosis Affecting the Spine
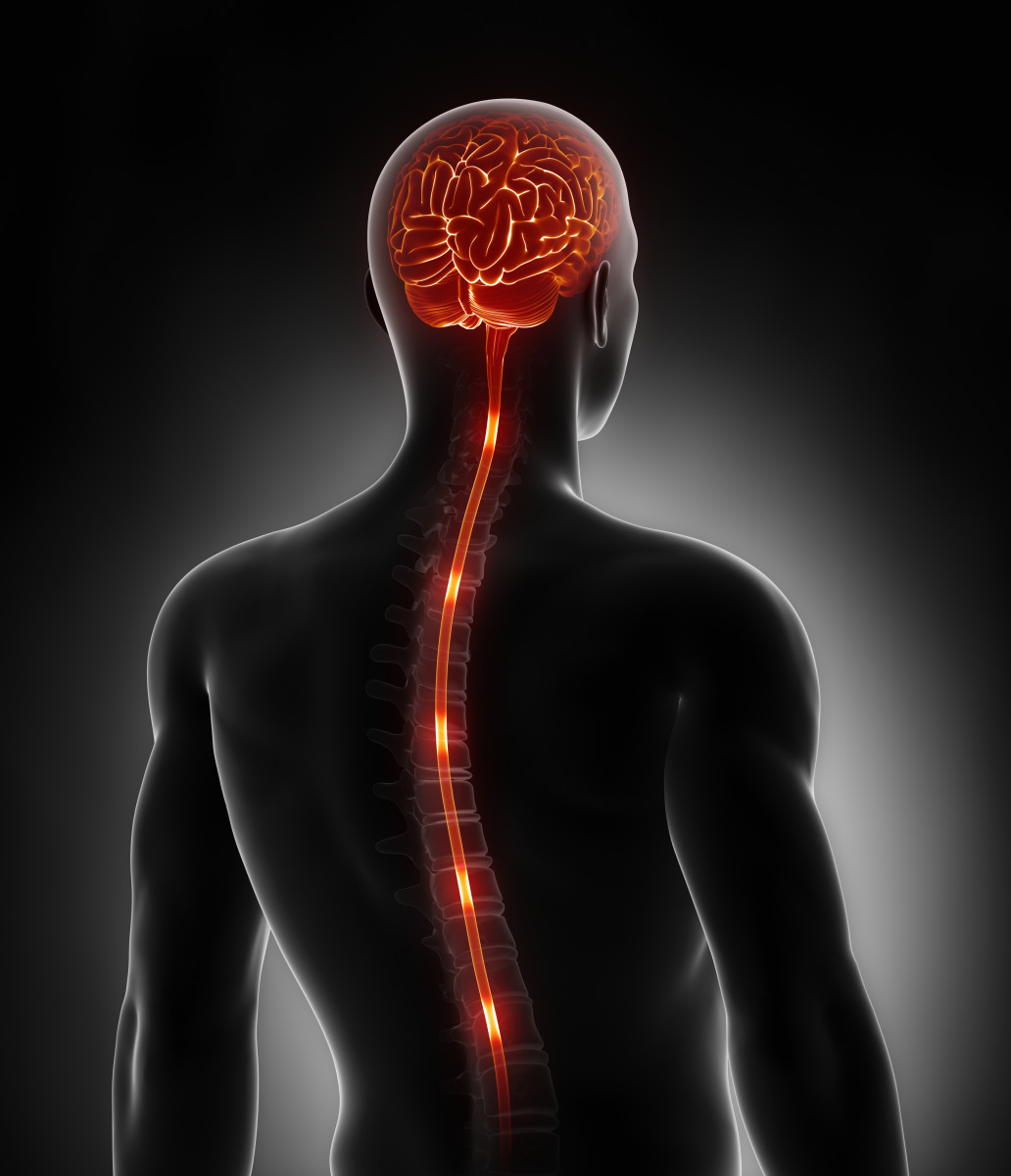
Sarcoidosis affecting the spinal cord tends to result in distinct patterns visible on MRIs of the spine, which may help in properly diagnosing this disease type, a new study reports.
The study, “Clinical and MRI phenotypes of sarcoidosis-associated myelopathy,” was published in the journal Neurology Neuroimmunology & Neuroinflammation.
The nervous system is affected in about 5% of sarcoidosis patients. Sometimes, this can manifest as damage to the spine, referred to as sarcoidosis-associated myelopathy (SAM). However, diagnosing SAM can be challenging because its symptoms and signs — including features visible on an MRI scan — can overlap with those of other spinal cord disorders.
A better understanding of features specific to SAM are needed, particularly because SAM is easier to treat than many other spinal disorders (e.g., tumors).
Researchers at the Johns Hopkins Hospital reviewed data from patients diagnosed with SAM to better determine the clinical and spinal MRI characteristics of the disease.
They analyzed data from 62 people diagnosed at the Johns Hopkins Myelitis and Myelopathy Center. The average age of this group was 47, 33 were male (53%), and 30 were African American (48%). SAM was the first clinical presentation of sarcoidosis in 49 patients (79%).
In 81% of these people, the symptoms of SAM were chronic, and the most frequent — reported in 54 people (87%) — were sense abnormalities.
“Clinically, we have shown that SAM typically has a chronic temporal evolution dominated by sensory symptoms,” the researchers wrote.
The fluid that surrounds the brain and spinal cord — known as the cerebrospinal fluid (CSF) — was analyzed in 4 of these patients. Results showed elevated immune cell counts (pleocytosis) in 34 people (79%), and abnormally high protein levels in 32 (74%).
“Our study showed that CSF studies in SAM typically reveal nonspecific markers of inflammation (i.e., pleocytosis and elevated protein),” the researchers wrote.
Four patterns of MRI features were noted. The most common was longitudinally extensive myelitis — that is, lesions that extend over three or more vertebrae — detected in 28 people (45%).
Other relatively common MRI patterns included short tumefactive myelitis (tumor-like lesions) and spinal meningitis (with inflammation of the membrane around the spine predominantly affected). Each of these types were identified in 14 individuals (23%).
In six people (10%), a pattern of inflammation was seen at places of disc degeneration, the ‘wear-and-tear’ of the discs that help to cushion each vertebrae.
In combination with previous research, these findings suggested that longitudinally extensive myelitis “can be considered the classic imaging phenotype of SAM,” the researchers wrote. “However,” they added, “given that this MRI lesion pattern was only present in 45% of our cohort, our description of other distinct imaging phenotypes occurring in SAM is of particular importance.”
Of note, in 26 patients, inflammation was predominantly seen in parts of the spinal cord that are subject to mechanical stress.
“We interpret these observations as suggesting that the inflammation of SAM may have a predilection for areas of the spinal cord susceptible to mechanical stress, potentially providing clues to the pathophysiology of this condition,” the researchers wrote.
These findings outline how SAM tends to manifest, particularly with regard to MRI findings. “Through detailed neuroimaging review of a large number of cases, we have identified a number of characteristic lesion patterns … potentially aiding physicians in the recognition and diagnosis of SAM,” the team added.
Future studies are needed “to explore lesion evolution and how this correlates with clinical outcomes,” it concluded.