Neurosarcoidosis Linked to Spinal Inflammation, Fluid in Brain in Case Report
Written by |
Although neurological symptoms are rare in people with sarcoidosis, physicians should consider neurosarcoidosis in cases of myelitis and hydrocephalus, as prompt steroid treatment can improve patient outcomes.
The recommendation comes from researchers at the Jersey Shore University Medical Center in a recent case study, “Hydrocephalus and myelopathy: A rare and challenging case of sarcoidosis and a review of literature,” published in the journal Clinical Case Reports.
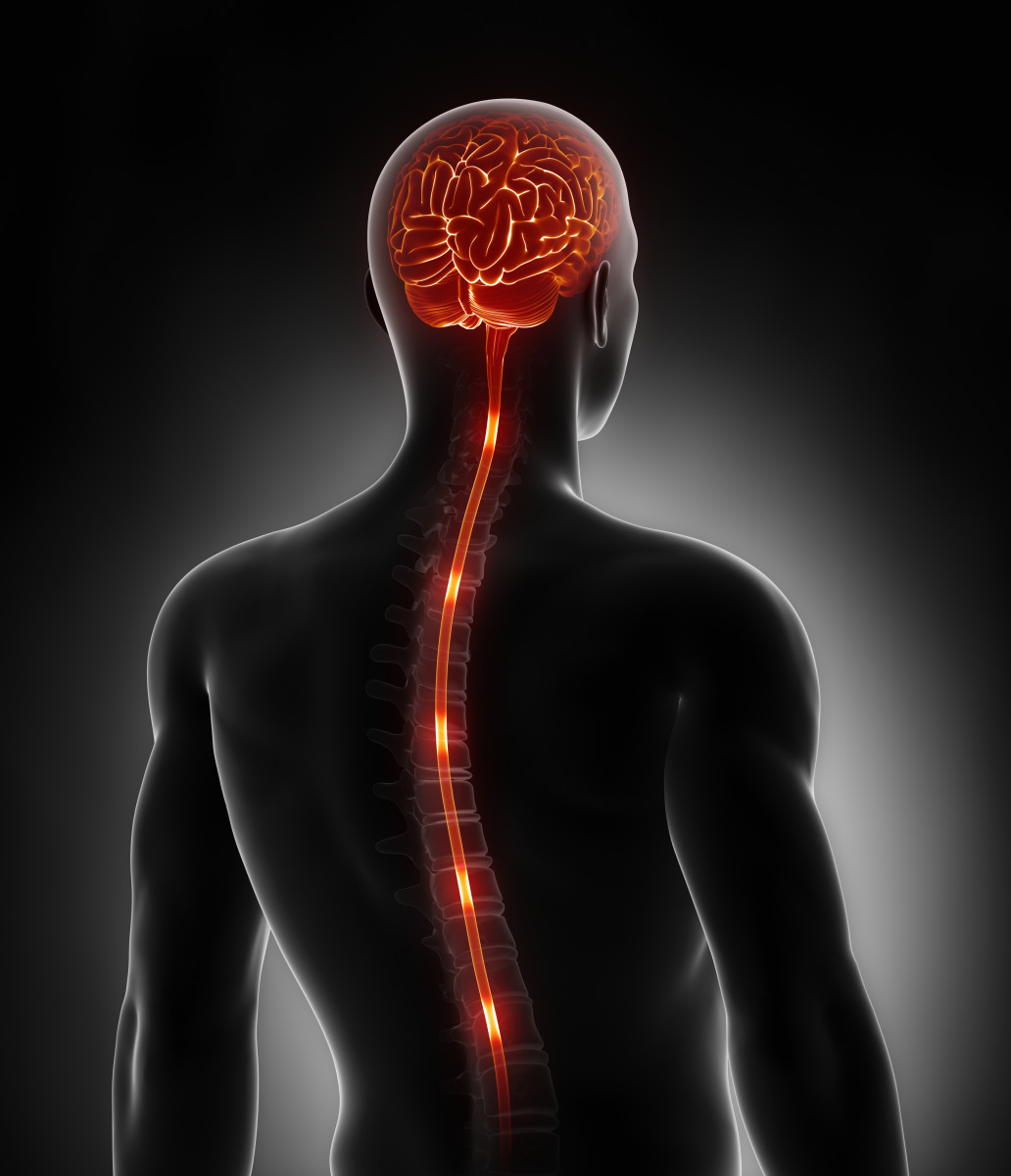
Sarcoidosis is characterized by clumps of inflammatory immune cells called granulomas that form on certain tissues and affect how those tissues work. Roughly 5% to 15% of sarcoidosis patients develop neurosarcoidosis, where granulomas form in either the central nervous system — the brain and spinal cord — or along peripheral nerves.
Neurosarcoidosis can affect any part of the nervous system. But its two rarest manifestations are hydrocephalus, where cerebrospinal fluid (CSF) builds in cavities — called ventricles — deep within the brain, and myelitis, an inflammation of the spinal cord.
Neurosarcoidosis is often difficult to diagnose, given its rarity and because symptoms can be broad and atypical.
In the present case, a 38-year-old African-American man came to the center’s emergency department complaining of weakness in his left leg.
The patient described his leg as feeling numb and heavy, and said this sensation slowly progressed to both legs, before ascending into the body. He had no significant medical or family history, was mentally alert, and his vital signs all appeared within normal ranges.
Cardiology, pulmonary, gastrointestinal, and neurological examinations showed nothing unusual, and a skin exam revealed no rashes.
Notably, the man had been admitted to the hospital less than a year ago, complaining of headaches and confusion. He was diagnosed with acute communicating hydrocephalus, meaning that CSF was accumulating in his brain but was able to drain to some degree.
At the time, physicians drained the fluid by inserting a ventriculoperitoneal shunt and the man was soon discharged.
During this second hospital admission, the man began to develop urinary retention, or an inability to urinate, and a Foley catheter was inserted into his bladder.
Computerized tomography (CT) head scan showed neither obstructed blood vessels nor bleeding. Ventricles in the brain appeared stable in size.
An MRI scan revealed the presence of small nodules, or lumps, along the spinal cord of the lower back. A lumbar puncture, used to obtain CSF samples, found this fluid was clear, although with a high white blood cell count.
A chest X-ray revealed patchy spots on the patient’s upper right lung, and a chest CT scan found enlarged mediastinal and hilar lymph nodes, as well as signs of multiple nodules mostly in the upper right lung. A lymph node biopsy showed the presence of a number of cell types indicative of inflammation.
The patient’s sensation of numbness worsened progressively during his stay, reaching his waist. While the weakness in his legs also grew worse, he continued to maintain full strength in his upper extremities.
Taken together, the evidence supported neurosarcoidosis as the most likely diagnosis, although cancer remained a consideration, the team reported.
The patient refused a spinal cord biopsy, which could have confirmed a neurosarcoidosis diagnosis.
He was given a course of steroids and discharged to a rehabilitation facility on a slow oral prednisone taper.
At a follow-up appointment several months later, he reported some easing of numbness, but continuing leg weakness. He reported no worsening of his overall neurological symptoms.
A review of the medical literature revealed a few cases of neurosarcoidosis with either myelitis or hydrocephalus, although none with both conditions without a previous diagnosis of sarcoidosis.
This patient’s symptoms were similar to those reported in past cases, but response to treatment differed in each case.
Given such variability in symptoms and responses, and the lack of any standardized diagnostic criteria for neurosarcoidosis, the team recommended that sarcoidosis be considered in cases like this one, where other conditions have been excluded.
“Although we have insufficient randomized controlled trials guiding NS [neurosarcoidosis] treatment, early diagnosis, timely treatment with steroids, and a referral to a specialist center can be associated with a favorable outcome and prevent further deterioration and long-term disability,” the researchers wrote.
Further research into this area is needed, they emphasized.





