Case Analysis Sheds Light on Bidirectional Ventricular Tachycardia in Cardiac Sarcoidosis
A new report discussing the case of a cardiac sarcoidosis patient with bidirectional ventricular tachycardia (BVT) provides additional information to help improve diagnoses in these patients.
The study, “Bidirectional ventricular tachycardia in cardiac sarcoidosis,” was published in the Journal of Arrhythmia.
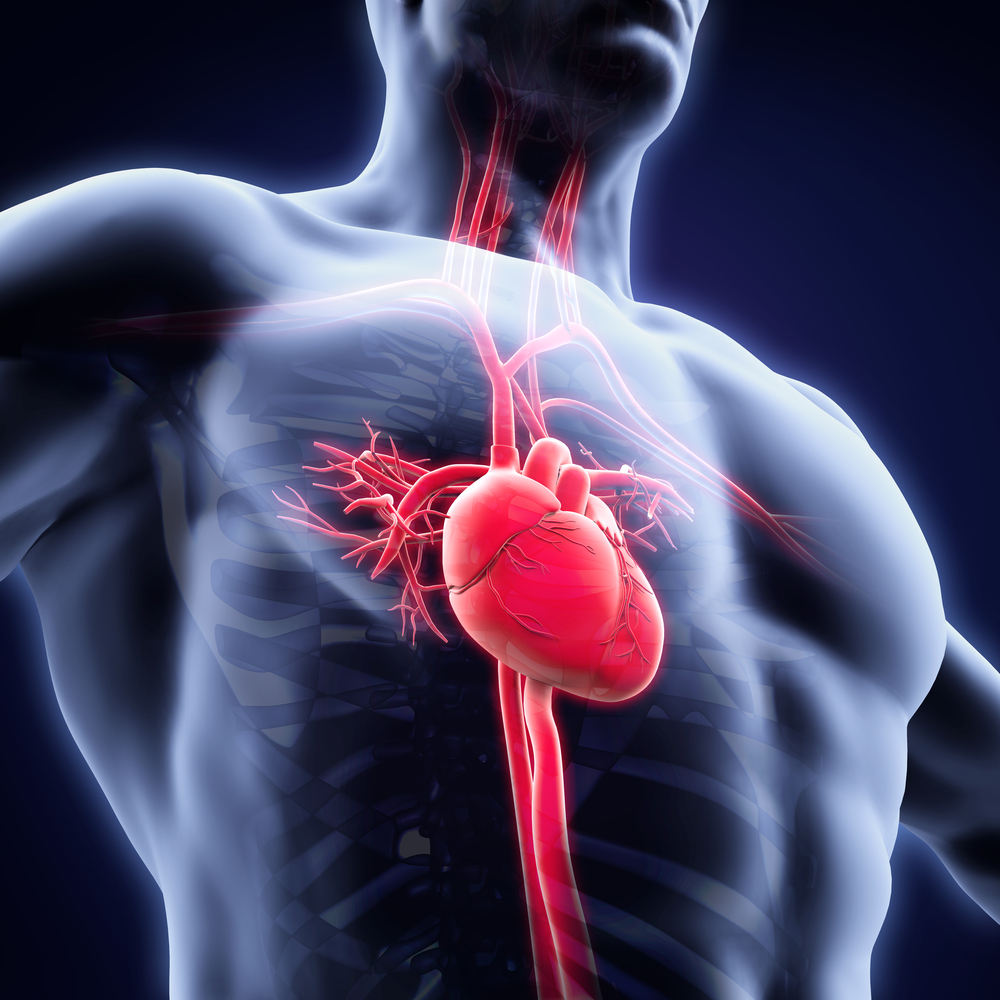
Cardiac sarcoidosis involves myocardial inflammation and fibrosis (tissue scarring), which may lead to impaired heart function and the occurrence of abnormal heart rhythm, called arrhythmias. BVT, characterized by a heart rate of 140-180 beats per minute, is among the cardiac complications observed in sarcoidosis patients.
A research team led by Mina M. Benjamin, MD, from the Department of Internal Medicine at the University of Wisconsin Hospital and Clinics, reported and discussed a case of BVT in a 73-year-old man with cardiac sarcoidosis.
The patient had a history of pulmonary sarcoidosis and was found to have non-sustained BVT. The results of cardiac magnetic resonance revealed patchy alterations in the left ventricular myocardium, consistent with the diagnosis of cardiac sarcoidosis. The possibility of ischemia, or insufficient blood supply, was ruled out.
Follow-up analysis one year later revealed disease progression, which prompted the start of immunosuppression therapy to reduce the impact of arrhythmias. The patient also was elected to receive a defibrillator implant to prevent sudden cardiac death.
“This surgery was recommended due to the high burden of non-sustained VT episodes, left and right ventricular dysfunction, and the presence of fibrosis and active inflammation by imaging studies,” the authors wrote. “Implantation for primary prevention is commonly performed due to the high burden of VT events (estimated incidence rate of 15% per year) in patients with cardiac sarcoidosis.”
Previous studies reported variable success in the ablation, or surgical removal of tissue, of VT in patients with cardiac sarcoidosis. In the present case, the team found a scar-mediated focus in the septum, which can lead to alternate blood passage into the right or left ventricle, ultimately complicating the elimination of arrhythmias. The authors argue that this may be the mechanism explaining the presence of BVT in this patient.
Although the alteration in the septum was only detected one year after initial diagnosis, the authors do not rule out its earlier presence, which may have been microscopic and undetectable.
According to the team, physicians should keep in mind that “BVT may indicate septal involvement with sarcoidosis before the lesions are large enough to be detected radiologically.”






