Certain Immune Cells May Drive Sarcoidosis by Producing Inflammatory Agents, Study Suggests
Written by |
Intermediate monocytes, a type of immune cell, may contribute to the development and progression of sarcoidosis through the production of TARC — a molecule that attracts other specific immune cells linked to inflammation, according to a small study.
These findings point to intermediate monocytes and TARC as potential treatment targets for sarcoidosis.
The study, “Circulating intermediate monocytes produce TARC in sarcoidosis,” was published in the journal Allergology International.
Sarcoidosis is a highly heterogeneous inflammatory disease that leads to the formation of small abnormal lumps or nodules of inflammatory cells — called granulomas — in several organs, ultimately affecting how well they work.
While sarcoidosis’ underlying mechanisms are still unclear, evidence suggests that chemotactic molecules — those that promote directional movement of cells toward its source — may contribute to the formation of granulomas by attracting and immobilizing immune cells at affected sites.
In a previous study, Japanese researchers found that people with sarcoidosis have high levels of a chemotactic molecule called thymus- and activation-regulated chemokine (TARC) in the blood and within skin granulomas. TARC levels were also associated with disease severity in these patients.
TARC — also known as CCL17 — attracts a type of immune cell, called Th2, into inflammation sites and induces Th2 activation, which is associated with allergy, inflammation, and scarring (fibrosis) when unbalanced.
“The [production] of TARC within granulomas and its presence in the circulation may suggest that TARC plays some key roles in driving the immune response toward a Th2 environment in sarcoidosis,” the researchers wrote.
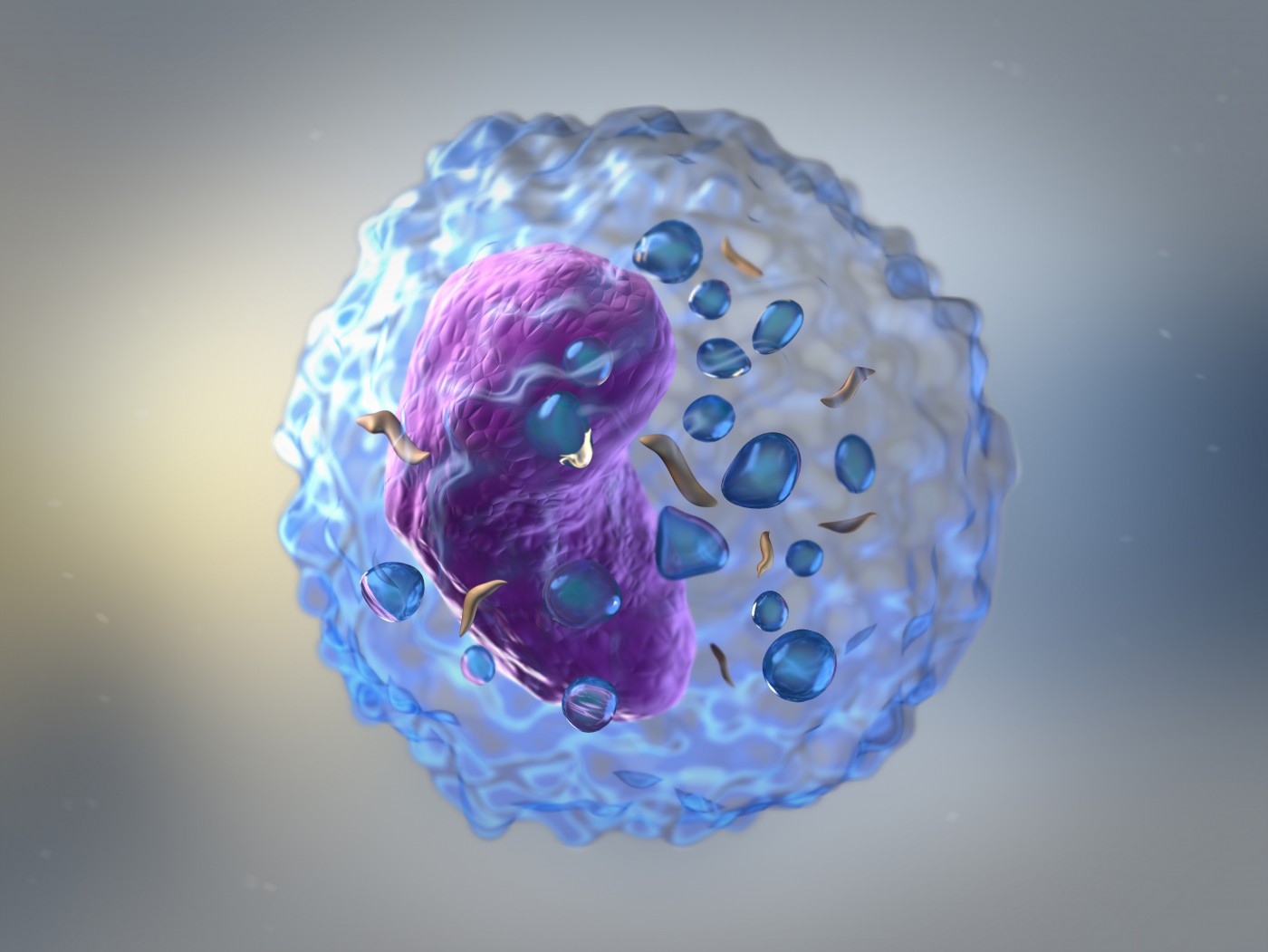
Previous work indicated that monocytes — a type of immune cell that is rapidly recruited to sites of infection and inflammation — were a source of TARC in circulating blood.
Moreover, a study in mice showed that intermediate monocytes, a subtype of monocytes, migrate into tissues, drive local inflammatory responses, and produce high levels of TARC. Interestingly, intermediate monocytes have been found in high numbers in people with inflammatory diseases, including sarcoidosis.
This same team of Japanese researchers now set out to evaluate the potential role of circulating intermediate monocytes in sarcoidosis by measuring their ability to produce TARC.
The researchers analyzed the proportion of each monocyte subtype (classical, intermediate, and non-classical), and their respective production of TARC in 13 sarcoidosis patients (seven women and six men). These values were compared with those found in samples from nine healthy volunteers.
Patients’ mean age was 71, and they had lived with the disease for a mean of 6.1 years. Based on chest radiography evaluation, most were considered to have mild disease.
Results showed that while people with sarcoidosis had similar numbers of circulating monocytes compared to healthy people, they showed a significantly higher proportion of circulating intermediate monocytes.
Patients’ intermediate monocytes also produced significantly higher levels of TARC than the two other subtypes, and there was a significant association between the proportion of circulating intermediate monocytes and TARC blood levels.
Researchers concluded that their findings suggest that higher numbers of circulating intermediate monocytes with more potential to produce TARC may contribute to the development of sarcoidosis.
“The identification of TARC-producing intermediate monocytes in circulation suggests that these expanded pro-inflammatory cells could enter into affected tissue, and could be crucial for building and maintaining granuloma formation,” they wrote.
They noted, however, that future studies are required to confirm this hypothesis.
“This finding highlights the important role of this inflammatory monocyte subset, and should lead to additional studies focusing on their exact function in the [development] of this challenging disease,” the team added.





