Monocytes, a Specific Immune Cell, Linked to Inflammation in Sarcoidosis
Lower expression of a receptor at the surface of immune cells, called monocytes, in the blood of sarcoidosis patients is linked to disease development.
The study “Reduced expression of monocyte CD200R is associated with enhanced proinflammatory cytokine production in sarcoidosis” was published in the journal Scientific Reports.
Sarcoidosis is an inflammatory disease affecting multiple organs, but its most common manifestation is pulmonary sarcoidosis.
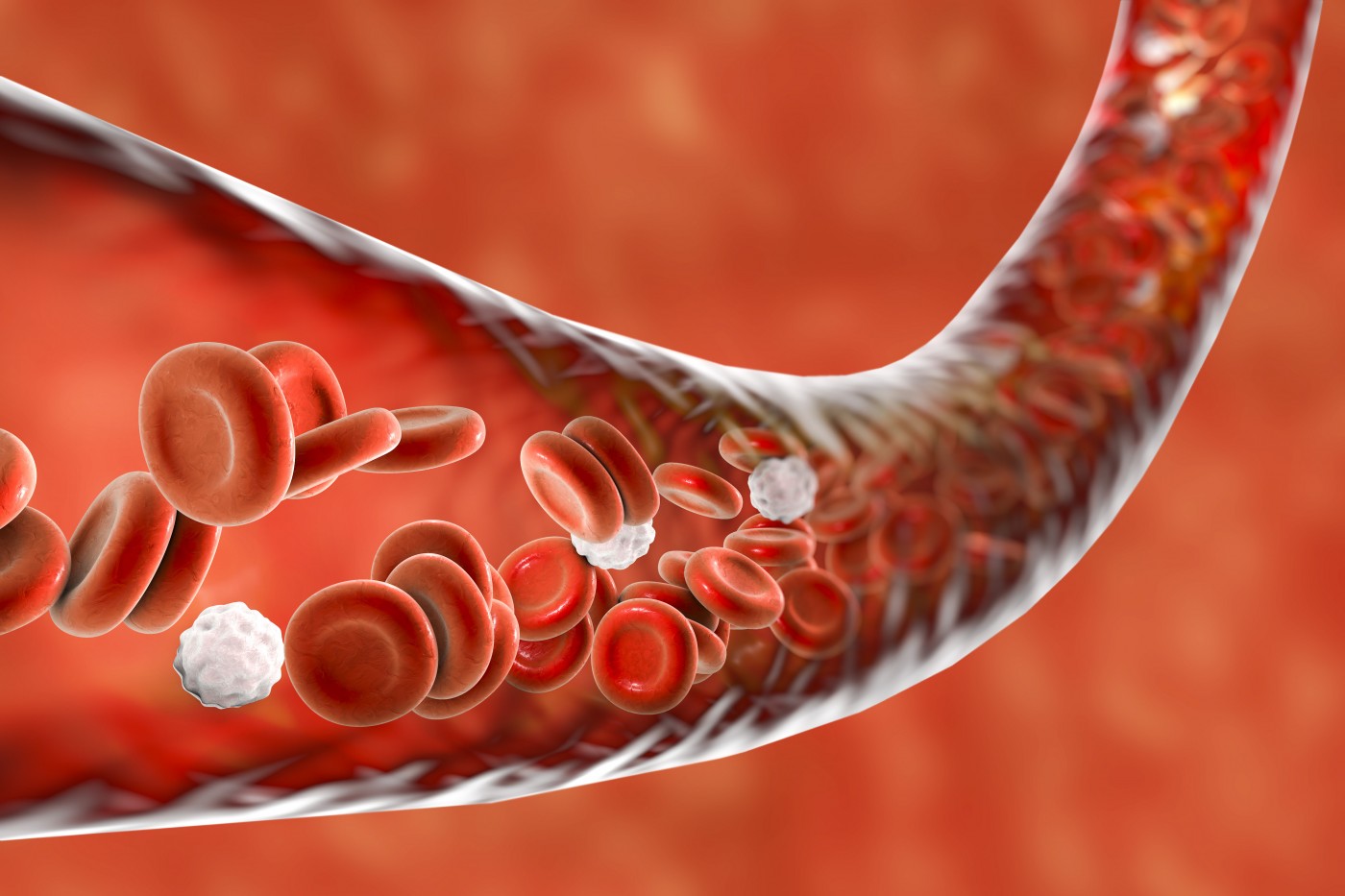
Immune cells in the lungs, particularly monocytes and lymphocytes (both belong to the large family of white blood cells), are major producers of pro-inflammatory cytokines, such as tumor necrosis factor (TNF) and interleukin-6 (IL-6). Regulating the inflammatory responses mediated by these cells and associated cytokines is crucial to prevent tissue damage in sarcoidosis.
Immune cells carry receptors that are capable of modulating the production of cytokines. Lower expression of specific receptors is linked to tissue inflammation.
In this study, a team of researchers investigated the role of such receptors in monocytes circulating in the blood of patients with sarcoidosis.
They measured the amount of cytokines that are released from circulating immune cells after whole blood was stimulated with phytohaemagglutinin, or PHA (PHA has the capacity of activating a wide range of immune cells).
Researchers observed that TNF and IL-6 released from PHA-stimulated whole blood was greater in patients with sarcoidosis when compared to healthy people. They then identified monocytes as the cells responsible for the enhanced cytokine production observed in sarcoidosis patients.
TNF secretion by monocytes and macrophages (another type of immune cell) is regulated by several receptors sitting at the cells’ surface. Analyzing the expression of some of these receptors in blood monocytes, authors found that the expression of the receptor called CD200R was reduced in patients with sarcoidosis. They found that 52.9% of sarcoidosis patients showed low levels of CD200R (and were classified as CD200Rlow), while this number was only 11.7% in healthy controls.
In addition, researchers observed that CD200Rlow phenotype was associated with increased pro-inflammatory cytokine release, specifically shown by higher production of TNF and IL-6 in response to PHA stimulation.
When the team blocked the expression of this receptor in healthy donors (thereby inducing a decrease in the receptor’s expression), they observed that monocytes of healthy controls started to increase the secretion of TNF and IL-6. This shows that just by blocking the receptor, researchers were able to reproduce the hyper-activated state of monocytes detected in sarcoidosis patients.
These results support a potential role for blood monocytes as important regulatory cells in sarcoidosis. The suggested mechanism may be linked to the CD200R receptor regulatory role of pro-inflammatory cytokine release from monocytes in sarcoidosis patients. Therefore, the team suggests that a future therapeutic strategy for sarcoidosis may include modulating CD200R receptor expression.