Abnormal activation of immune cells, fibroblasts seen in granulomas
Experimental treatment was able to reduce granuloma formation in mouse model
Researchers have uncovered a network of abnormally activated immune cells and fibroblasts — the primary active cell of connective tissue — within granulomas, the clumps of cells that cause sarcoidosis.
The key players in granuloma formation include metabolically reprogrammed immune macrophages, immune T-helper (Th) cells producing pro-inflammatory molecules, and fibroblasts with inflammatory and tissue-altering characteristics.
In addition, researchers discovered a way to attenuate granuloma formation in a mouse model of sarcoidosis by using an investigational medicine to block a macrophage-produced protein involved in tissue remodeling and immune activation.
“We anticipate that our dataset and methodology can help [identify] promising strategies for interfering with granuloma formation in sarcoidosis,” they wrote.
The study, “Single-cell and spatial transcriptomics reveal aberrant lymphoid developmental programs driving granuloma formation,” was published in the journal Immunity.
Granulomas can contribute to diseases like sarcoidosis
Granulomas, complex structures of immune and structural cells, “form in response to infections by bacteria and fungi, but they also contribute to diseases such as sarcoidosis,” causing tissue scarring and organ damage, the researchers wrote.
Sarcoidosis is characterized by the abnormal formation of granulomas in various organs and tissues, most commonly the lungs and lymph nodes, which work as filters for foreign substances. Granulomas may also form in the eyes, skin, and liver, leading to a range of symptoms.
However, the molecular and cellular processes behind granuloma formation are still unclear.
To learn more, researchers in Austria conducted a detailed analysis of skin samples, with and without granulomas, from 12 adults (eight women and four men) with active chronic skin sarcoidosis. Their median age was 54 years.
The team applied single-cell RNA sequencing, a method to measure gene activity in individual cells, and spatial transcriptomics, a technique to identify cell types and their locations within tissue samples.
Based on gene activity profiles, seven non-immune (mainly structural cells) cell clusters and 13 immune cell clusters were observed in both skin samples with and without granulomas.
However, macrophages, Th cells, and fibroblasts “were almost exclusively found” in granuloma-containing skin, the team wrote, with additional experiments placing them mostly inside granulomas. Each of the three cell types had unique gene activity signatures compared with the surrounding unaffected skin.
These gene activity patterns were consistent with those reported in previous studies for lung granulomas, “indicating that certain regulatory pathways of granuloma formation are shared across organs,” the researchers wrote.
In the skin, macrophages normally remove microbes and debris from infected and dead cells. Granuloma-associated macrophages, however, had an abnormal gene activity signature that promoted inflammation, immune processes, energy generation, metabolism, and organization of the extracellular matrix (ECM). ECM is a network of molecules that provides scaffolding for cells.
A particular subset of these cells, exclusively located in granulomas, showed high activity of several sarcoidosis-related genes, inflammation-promoting genes, and genes coding for matrix metalloproteinases (MMPs), which are enzymes involved in ECM breakdown.
“These macrophages support … immune responses and ECM remodeling, thereby contributing to a microenvironment of persistent inflammation in granulomas,” the researchers wrote.
We anticipate that our dataset and methodology can help [identify] promising strategies for interfering with granuloma formation in sarcoidosis.
Granuloma-associated Th cells contain pro-inflammatory molecular signature
Consistently, granuloma-associated Th cells appeared to have acquired a molecular signature, called Th17.1, “that promotes macrophage activation and inflammation,” the team wrote.
Notably, Th17.1 cells were previously detected in the lung fluid of pulmonary sarcoidosis patients, “indicating similar T cell responses in granulomas of other organs,” they added.
Structural cells, such as fibroblasts and endothelial cells, provide metabolic support and shape to tissues and organs.
Endothelial cells are those that line blood and lymphatic vessels. The lymphatic system works as a communication route between tissues and the immune system, with the drained lymphatic fluid from body tissues, including the skin, being filtered at lymph nodes.
Within granulomas, two subsets of fibroblasts were identified. Immune-interacting fibroblasts showed increased activity of genes involved in pro-inflammatory responses, cell recruitment and retention, attraction and activation of macrophages, immune processes, and cellular communication.
Tissue-remodeling fibroblasts were characterized by increased gene activity related to both components and regulators of ECM.
Granuloma-associated endothelial cells showed more subtle gene profile differences to those in non-affected skin. Still, these were associated with “ECM remodeling … and cell migration from the circulation into the granulomas,” the team wrote.
Granuloma-associated macrophages, T-cells, and fibroblasts all produced molecules involved in cellular communication, suggesting they all communicate within the granuloma environment. Beyond this cellular crosstalk, genes that control structural interactions and binding support to neighboring cells were identified.
Overall, these findings indicated that abnormal macrophages promote an inflammatory microenvironment and attract structural cells and other immune cells that, in turn, further boost macrophage activation.
Also, fibroblasts “appear to shape the structure of granulomas by regulating the ECM together with macrophages,” the team wrote, adding that altered ECM “may create tracks for cell migration that guide immune cells inside the granulomas.”
Four weeks of experimental treatment reduced granuloma-induced skin swelling
The team also found similarities between granulomas and tertiary lymphoid structures, which form in non-lymphoid tissues close to tumors or sites of infection and contribute to effective immune responses.
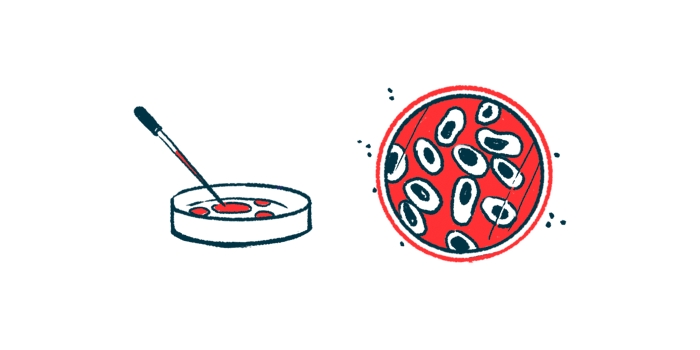
To explore the therapeutic potential of these data, the researchers used an experimental treatment to suppress the activity of MMP12 in a mouse model of sarcoidosis. MMP12 is an ECM-breakdown enzyme whose production was markedly elevated in granulomas-associated macrophage and was previously found in granulomas from several organs.
Four weeks of the MMP12 inhibitor significantly reduced granuloma-induced skin swelling in the mouse model, compared with untreated mice.
“These results support a functional contribution of matrix metalloproteinases in granuloma formation and maintenance, likely mediated by their role as ECM modulators and immune cell activators,” the team wrote.
“Our analyses establish an integrated molecular and spatial landscape of non-infectious granulomas and provide a rich dataset for therapeutic targeting of the biological processes underlying granuloma formation,” the researchers concluded.