Tuberculosis-causing Bacteria Linked to Sarcoidosis, Study Confirms
The bacteria that causes tuberculosis, Mycobacterium tuberculosis, is also involved in sarcoidosis development, a study has confirmed.
This knowledge may help doctors better diagnose sarcoidosis and other systemic inflammatory diseases, and perhaps lead to immunotherapies against them.
The study, “Humoral immune profiling of mycobacterial antigen recognition in sarcoidosis and Löfgren’s syndrome using high-content peptide microarrays,” was published in the International Journal of Infectious Diseases.
Researchers led by Dr. Markus Maeurer of Sweden’s Center for Allogeneic Stem Cell Transplantation (CAST) tested blood samples from people with sarcoidosis, Löfgren’s syndrome — an acute form of sarcoidosis — and tuberculosis. The team also included healthy controls in the testing at Karolinska University Hospital, where the center is based.
They were specifically looking for the presence of antibodies against Mycobacterium tuberculosis.
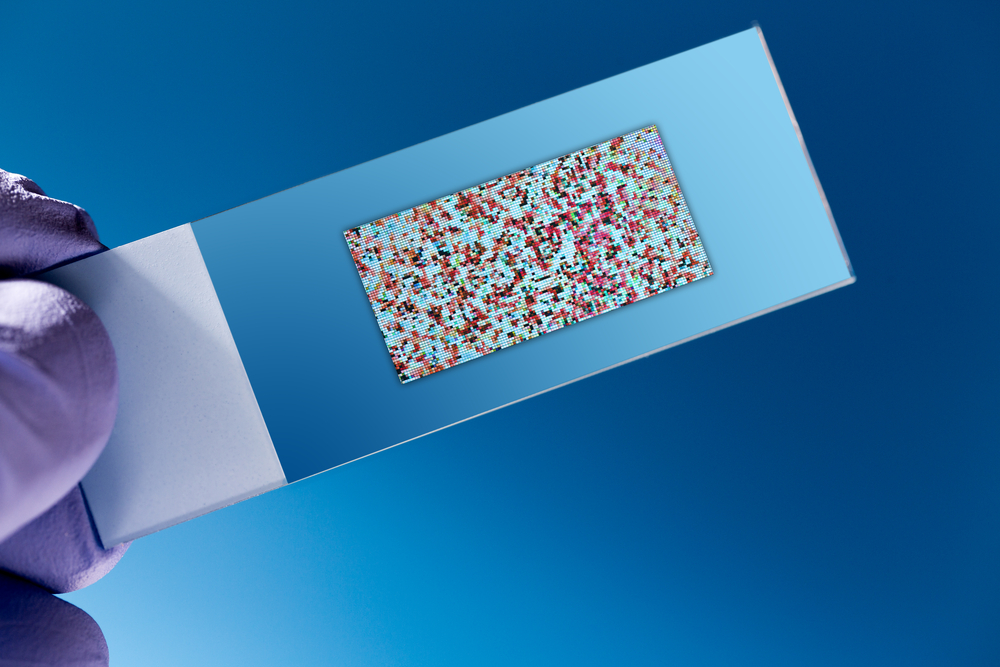
Researchers used a technique called high-content peptide microarrays (HCPM) to spot 5,964 peptides on microscope slides. The peptides spanned 145 known M. tuberculosis proteins.
Daubing patients’ serum on the slides allowed researchers to identify all of the antibodies the body can produce against different M. tuberculosis peptides. The presence of an antibody against a bacteria-specific peptide indicates an infection with that bacteria.
Researchers found specific antibody responses against M. tuberculosis antigens in the serum of all study groups — patients with either sarcoidosis, Löfgren’s syndrome, or tuberculosis, or controls.
When the research team compared the three disease groups with controls, they found the serum from sarcoidosis patients recognized 258 peptides, the serum from Löfgren’s syndrome patients recognized 313 peptides, and the serum from tuberculosis patients recognized 147 peptides. Detailed analysis revealed specific patterns of recognition for each condition and for the controls.
The presence of the patterns raises the possibility of using a blood sample to diagnose sarcoidosis, the researchers said. The current approach is examining bronchoalveolar lavage fluid. It is obtained by passing a tube through the nose or mouth into the lungs, squirting a fluid into the lungs, then extracting the fluid for examination.
Since the immune response between patients with sarcoidosis and tuberculosis is different, researchers speculate that genetic factors may determine how the body responds to an M. tuberculosis encounter. The kind of response may then determine whether the body is able to control bacterial growth or whether sarcoidosis or tuberculosis will develop.
“The antibody responses to the M. tuberculosis antigens discussed in this study have not been described before for patients with sarcoidosis or Löfgren’s syndrome, which also largely applies to TB [tuberculosis] patients. Taken together, the findings presented in this report shed new light on an array of mycobacterial epitopes, i.e., antigens that may have significance in the pathogenesis of sarcoidosis and associated systemic inflammatory diseases,” the team wrote. “This, therefore, opens up new possibilities for improving our understanding of the immunology that sustains granulomatous inflammation and may also assist in the development of non-invasive diagnostics.”
“Specific IgG [antibody] recognition patterns for M. tuberculosis antigens in sarcoidosis patients re-affirm mycobacterial involvement in sarcoidosis, providing biologically relevant targets for future studies pertaining to diagnostics and immunotherapy.” the researchers wrote.